Arthritis Medicines: Understanding Your Treatment Options:-
Category Overview:-
Arthritis medicines represent a diverse group of treatments designed to help manage joint inflammation, reduce pain, and improve mobility in people living with various forms of arthritis. Healthcare professionals prescribe or recommend these medicines to address the underlying inflammation that causes joint damage, while also providing symptom relief that allows patients to maintain their daily activities and quality of life.
These treatments range from over-the-counter pain relievers to prescription disease-modifying medications, each serving specific roles in arthritis management. Doctors select appropriate medicines based on the type of arthritis diagnosed, the severity of symptoms, the joints affected, and individual patient factors such as age, overall health, and response to previous treatments.
Conditions Treated:-
Medicines in this category are used to manage several types of arthritis and related inflammatory joint conditions:
Osteoarthritis is the most common form, occurring when protective cartilage cushioning the joints wears down over time, leading to pain, stiffness, and reduced joint function.
Rheumatoid arthritis is an autoimmune condition where the body’s immune system mistakenly attacks joint tissues, causing inflammation, swelling, and potential joint deformity if left unmanaged.
Psoriatic arthritis affects some people with the skin condition psoriasis, causing joint inflammation alongside skin symptoms.
Ankylosing spondylitis primarily affects the spine and can lead to stiffness and reduced flexibility in the back.
Gout results from uric acid crystal buildup in joints, causing sudden, severe pain episodes.
These medicines may also be prescribed for other inflammatory joint conditions as determined appropriate by healthcare providers.
Types of Medicines in This Category:-
Arthritis treatments are organized into several therapeutic approaches:
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) are available both over-the-counter and by prescription, working to reduce inflammation and relieve pain. These come in oral tablets, capsules, and topical preparations.
Disease-Modifying Antirheumatic Drugs (DMARDs) are prescription medicines that slow disease progression in inflammatory arthritis by affecting the underlying immune system processes. These include traditional oral medications and newer biologic therapies administered by injection or infusion.
Corticosteroids are powerful anti-inflammatory medicines available as oral tablets, injections directly into affected joints, or intravenous infusions for severe cases.
Analgesics focus primarily on pain relief without significant anti-inflammatory effects, ranging from simple over-the-counter options to stronger prescription formulations.
Topical treatments include creams, gels, and patches applied directly to painful joints, offering localized relief with reduced systemic effects.
Uric acid-lowering agents specifically target gout by reducing uric acid production or increasing its elimination from the body.
How These Medicines Work?
Arthritis medicines employ different mechanisms depending on their classification:
Anti-inflammatory medicines work by blocking specific enzymes or chemical messengers in the body that promote inflammation. By interrupting these inflammatory pathways, they reduce swelling, warmth, and pain in affected joints.
Disease-modifying medications target various components of the immune system that mistakenly attack joint tissues in autoimmune forms of arthritis. Some suppress overactive immune responses broadly, while biologic therapies target specific immune system proteins involved in inflammation.
Pain-relieving medicines affect how the nervous system processes pain signals, either at the site of discomfort or in the brain and spinal cord, providing relief without necessarily addressing inflammation.
Topical preparations penetrate skin layers to deliver active ingredients directly to affected areas, providing localized relief while minimizing absorption into the bloodstream.
The specific mechanism varies significantly between medicine types, which is why healthcare providers carefully select treatments based on the form of arthritis being managed and treatment goals.
Who May Benefit From This Category?
Healthcare providers may prescribe or recommend arthritis medicines for patients who:
– Have received a confirmed diagnosis of arthritis or a related inflammatory joint condition from a qualified healthcare professional
– Experience persistent joint pain, stiffness, or swelling that interferes with daily activities
– Show signs of disease progression that could lead to joint damage if left unmanaged
– Have not achieved adequate symptom control through non-medication approaches alone
– Require both symptom management and disease modification in inflammatory arthritis
The suitability of specific medicines depends on numerous individual factors, including the type and severity of arthritis, other existing health conditions, current medications, pregnancy status, and previous treatment responses. Only a healthcare provider can determine which treatment approach is appropriate for each person’s unique situation.
Important Safety Information:-
All arthritis medicines carry potential risks and require careful medical oversight:
Medical consultation is essential before starting any new arthritis medication. Self-diagnosis and self-treatment can lead to inappropriate medicine selection, delayed proper diagnosis, and potentially serious health complications.
Pre-existing health conditions may make certain arthritis medicines unsuitable. People with heart disease, kidney problems, liver conditions, stomach ulcers, bleeding disorders, or high blood pressure need particularly careful medicine selection and monitoring.
Pregnancy and breastfeeding considerations are critical, as many arthritis medicines can affect fetal development or pass into breast milk. Women who are pregnant, planning pregnancy, or breastfeeding must discuss treatment options thoroughly with their healthcare provider.
Drug interactions are common with arthritis medicines. Patients should inform their healthcare provider about all medications, supplements, and herbal products they take to avoid potentially dangerous combinations.
Infection risk increases with certain disease-modifying and biologic therapies that affect immune system function. Patients taking these medicines should promptly report signs of infection and may need to pause treatment during illness.
Regular monitoring through blood tests and medical appointments is often necessary, particularly with disease-modifying medications, to detect potential side effects early and adjust treatment as needed.
Usage Guidance (General):-
Proper usage of arthritis medicines varies significantly based on the specific medication prescribed:
Dosage is highly individualized and depends on factors including the type of arthritis, disease severity, body weight, kidney and liver function, and how well a patient tolerates and responds to treatment. Never adjust dosing without consulting your healthcare provider.
Timing of doses matters for optimal effectiveness and safety. Some medicines work best when taken with food to reduce stomach upset, while others should be taken on an empty stomach for proper absorption.
Duration of treatment ranges from short-term use during symptom flares to lifelong management for chronic inflammatory conditions. Disease-modifying medicines often require several weeks or months before their full benefits become apparent.
Administration techniques require proper instruction, particularly for injectable or infused medications. Healthcare providers or pharmacists should demonstrate correct injection techniques and answer questions about self-administration.
Missed doses should be handled according to specific medicine guidelines. Generally, take a missed dose as soon as remembered unless it’s nearly time for the next scheduled dose, but never double up to make up for missed doses without medical guidance.
Always follow the precise instructions provided by your prescribing healthcare provider and dispensing pharmacist, and contact them promptly if you have questions about your treatment regimen.
Side Effects & Risks (General Overview):-
Arthritis medicines can cause various side effects, though not everyone experiences them:
Common side effects often include stomach upset, nausea, indigestion, or headaches with NSAIDs and some DMARDs. Many topical treatments cause mild skin irritation at application sites. These effects are often temporary and may lessen as your body adjusts to the medicine.
Gastrointestinal risks are notable with NSAIDs, which can cause stomach ulcers, bleeding, or perforation, particularly with long-term use or in older adults. Taking these medicines with food and using protective stomach medications can reduce these risks.
Cardiovascular considerations include increased risks of heart attack, stroke, and high blood pressure with some NSAIDs, especially at higher doses or with prolonged use.
Kidney and liver effects can occur with various arthritis medicines, ranging from mild changes in function tests to more serious organ damage in rare cases. This is why regular monitoring is important for many treatments.
Immune system effects from disease-modifying and biologic therapies increase susceptibility to infections and may slightly raise certain cancer risks over long-term use.
Serious side effects requiring immediate medical attention include signs of allergic reactions (difficulty breathing, facial swelling, severe rash), symptoms of bleeding (black or bloody stools, persistent bleeding), severe abdominal pain, yellowing of skin or eyes, or signs of serious infection.
Report any new or worsening symptoms to your healthcare provider promptly. Many side effects can be managed through dose adjustments, supportive measures, or switching to alternative treatments.
Choosing the Right Medicine:-
Selecting appropriate arthritis treatment is a collaborative process between patient and healthcare provider:
Diagnosis determines treatment approach. The type of arthritis you have significantly influences which medicines are appropriate. Treatments effective for osteoarthritis may not work for rheumatoid arthritis, and vice versa.
Individual factors guide selection, including your age, overall health status, other medications you take, previous treatment responses, lifestyle considerations, and personal preferences regarding treatment format (oral, injection, topical).
Treatment goals vary between managing acute symptom flares, controlling chronic pain, preventing disease progression, and maintaining joint function. Your healthcare provider will recommend medicines aligned with your specific goals.
Start with safer options when appropriate. Many healthcare providers begin with treatments that have better-established safety profiles before progressing to more intensive therapies if needed.
Trial and adjustment are often necessary. Finding the most effective medicine with acceptable side effects may require trying different options or combinations, which is a normal part of arthritis management.
Pharmacist consultation provides valuable insights into how to take medicines correctly, what to expect, potential interactions with your other medications, and how to manage minor side effects.
Never select arthritis medicines based solely on online information, recommendations from non-medical sources, or what has worked for others. Professional medical evaluation ensures you receive appropriate, safe, and effective treatment for your specific situation.
Storage & Handling Advice:-
Proper storage maintains medicine effectiveness and safety:
Temperature requirements vary by medication. Most oral arthritis medicines should be stored at room temperature away from excessive heat and moisture, making bathrooms generally unsuitable storage locations. Some injectable biologics require refrigeration at specific temperatures.
Original containers should be used for storage unless you use a pharmacy-provided pill organizer. Original packaging protects medicines from light exposure and moisture while keeping important information readily accessible.
Childproof storage is essential in households with children or visiting youngsters. Store all medicines in locked cabinets or high locations out of sight and reach.
Expiration dates indicate when the potency can no longer be guaranteed. Dispose of expired medicines properly rather than using them, as they may be ineffective or potentially harmful.
Travel considerations require planning, especially for refrigerated medicines. Use appropriate cold storage methods, carry medicines in hand luggage during flights, and ensure you have adequate supplies plus extras for unexpected delays.
Injectable medicine handling requires particular attention to instructions regarding needle disposal, proper mixing if needed, and maintaining sterility to prevent infections.
Disposal of unused medicines should follow local guidelines. Many pharmacies and community programs offer medicine take-back services. Never flush medicines down toilets unless specifically instructed, and don’t discard them in household trash where children or pets might access them.
Consult your pharmacist if you have specific questions about storing your arthritis medicines properly.
Frequently Asked Questions?
How long does it take for arthritis medicines to start working?
The timeframe varies considerably depending on the type of medicine. Simple pain relievers and NSAIDs typically provide relief within hours. However, disease-modifying antirheumatic drugs often require several weeks to several months before their full benefits become noticeable. Some biologic therapies show initial improvements within weeks, while others take longer. Your healthcare provider can give you specific expectations for your prescribed treatment. Patience is important, as stopping effective medicines too soon because you don’t notice immediate dramatic changes can allow disease progression.
Can I take arthritis medicines with other medications?
Potential drug interactions are common with arthritis medicines, making it essential to inform your healthcare provider and pharmacist about everything you take, including prescription medicines, over-the-counter products, vitamins, supplements, and herbal remedies. Some combinations are unsafe, while others require dose adjustments or timing modifications. For example, certain arthritis medicines interact with blood thinners, blood pressure medications, diabetes treatments, and even some antacids. Never assume combinations are safe without professional confirmation.
Are over-the-counter arthritis medicines as effective as prescription options?
Over-the-counter NSAIDs and pain relievers are sufficient for many people with mild to moderate osteoarthritis and provide meaningful symptom relief. However, inflammatory forms of arthritis like rheumatoid arthritis typically require prescription disease-modifying medications to prevent joint damage and control disease activity. Prescription-strength versions of some medicines also provide higher doses that may be more effective for severe symptoms. Your healthcare provider will recommend the most appropriate treatment intensity based on your specific diagnosis and needs.
What should I do if I experience side effects from my arthritis medicine?
Contact your healthcare provider if you experience side effects. Don’t stop taking prescribed medicines without medical guidance, as sudden discontinuation of some treatments can cause problems. Minor side effects sometimes improve as your body adjusts, or they can be managed with supportive measures. Your healthcare provider might adjust your dose, change how you take the medicine, add protective medications, or switch you to an alternative treatment. Serious side effects like difficulty breathing, severe abdominal pain, signs of bleeding, or symptoms of allergic reactions require immediate medical attention.
Medical Disclaimer:-
This content is provided for educational and informational purposes only and is not intended as medical advice, diagnosis, or treatment recommendations. The information presented here describes general characteristics of arthritis medicines as a category and should not be used as a substitute for professional medical consultation, diagnosis, or treatment planning.
Every individual’s medical situation is unique. Arthritis encompasses numerous distinct conditions requiring different treatment approaches. What is appropriate for one person may be ineffective, unnecessary, or potentially harmful for another. Only qualified healthcare providers who have examined you, understand your complete medical history, and have access to appropriate diagnostic information can make proper treatment recommendations.
Always consult with your physician, rheumatologist, or other qualified healthcare provider before starting, stopping, or modifying any arthritis treatment. Discuss your specific symptoms, medical history, current medications, and concerns to receive personalized guidance appropriate to your situation.
In case of medical emergency, including symptoms such as severe chest pain, difficulty breathing, signs of stroke, or severe allergic reactions, seek immediate emergency medical care by calling emergency services or going to the nearest emergency department.
This information does not create a healthcare provider-patient relationship. We strongly encourage you to work closely with your healthcare team for ongoing arthritis management and to report any concerns or changes in your condition promptly.
The content on this page is current as of the date of publication, but may not reflect the most recent medical research, treatment guidelines, or product information. Always verify information with current, authoritative medical sources and your healthcare provider.
-
Cyclophil Me 25mg (Cyclosporine)
Active Ingredient Cyclosporine Manufacturer Biocon Limited Packaging 5 capsules in 1 strip, 6 capsules in 1 strip Strength 25mg, 50mg, 100mg Delivery Time 6 To 15 days SKU: Cyclophil Me 25mg (Cyclosporine) Price range: $21.00 through $200.00Cyclophil Me 25mg (Cyclosporine)
Price range: $21.00 through $200.00 -
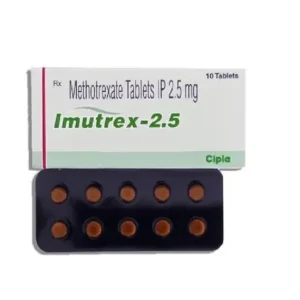
Imutrex 2.5 Mg (Methotrexate)
Active Ingredient Methotrexate Manufacturer Cipla Limited Packaging 10 tablets in 1 strip Strength 2.5 Mg, 7.5 Mg, 10 Mg Delivery Time 6 To 15 days SKU: Imutrex 2.5 Mg (Methotrexate) Price range: $27.00 through $195.00Imutrex 2.5 Mg (Methotrexate)
Price range: $27.00 through $195.00 -
Lefumide 10 Mg (Leflunomide)
Active Ingredient Leflunomide Manufacturer Cipla Limited Packaging 10 tablets in 1 strip Strength 10 Mg Delivery Time 6 to 15 days SKU: Lefumide 10 Mg (Leflunomide) Price range: $28.00 through $201.00Lefumide 10 Mg (Leflunomide)
Price range: $28.00 through $201.00