Rheumatoid Arthritis Medicines: Comprehensive Patient Guide:-
Rheumatoid arthritis Category Overview:-
Rheumatoid arthritis (RA) medicines represent a diverse group of treatments designed to manage this chronic autoimmune condition that causes inflammation, pain, and potential joint damage. Healthcare professionals prescribe these medications to reduce disease activity, slow progression, relieve symptoms, and help patients maintain their quality of life and physical function.
Modern RA treatment has evolved significantly, with doctors now able to offer multiple therapeutic options tailored to individual disease severity, patient response, and overall health status. These medicines work through various mechanisms to control the abnormal immune response that characterizes rheumatoid arthritis, and many patients require combination therapy for optimal disease management.
Rheumatoid arthritis Conditions Treated:-
Medicines in this category are primarily prescribed for:
Rheumatoid Arthritis: A chronic autoimmune condition where the immune system mistakenly attacks the body’s own joint tissues, causing inflammation, pain, swelling, and eventual joint damage if left untreated.
Associated Symptoms: These medications help manage joint pain, morning stiffness, swelling, reduced range of motion, fatigue, and systemic inflammation that can affect multiple body systems.
Related Autoimmune Conditions: Some medications in this category may also be prescribed for other inflammatory arthritis conditions, such as psoriatic arthritis, ankylosing spondylitis, or juvenile idiopathic arthritis, when determined appropriate by a rheumatologist.
Healthcare professionals diagnose rheumatoid arthritis through physical examination, blood tests measuring inflammatory markers and specific antibodies, and imaging studies. Treatment decisions are based on disease activity, progression risk, and individual patient factors.
Types of Medicines in the Rheumatoid Arthritis Category:-
Rheumatoid arthritis treatment includes several distinct types of medicine:
Disease-Modifying Antirheumatic Drugs (DMARDs): These are the cornerstone of RA treatment, working to slow disease progression and prevent joint damage. Conventional synthetic DMARDs like methotrexate are often first-line treatments, while targeted synthetic DMARDs offer more specific immune system modulation.
Biologic Response Modifiers (Biologics): These advanced medications target specific components of the immune system responsible for inflammation. They include TNF inhibitors, IL-6 inhibitors, B-cell depleting agents, and T-cell activation blockers, typically administered by injection or infusion.
JAK Inhibitors: A newer class of oral medications that block specific enzymes involved in the inflammatory process, offering an alternative for patients who don’t respond to or cannot tolerate biologics.
Corticosteroids: Short-term or low-dose oral steroids used to quickly reduce inflammation during disease flares or while waiting for DMARDs to take effect.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These provide symptomatic relief from pain and inflammation but do not modify disease progression.
Analgesics: Pain relief medications that may be used alongside disease-modifying treatments for additional comfort.
How These Medicines Work?
Rheumatoid arthritis medications function through different mechanisms depending on their class:
Immune System Modulation: DMARDs and biologics work by dampening or redirecting the overactive immune response that attacks joint tissues. Rather than suppressing the entire immune system, many modern medications target specific inflammatory pathways, helping to restore a more balanced immune function.
Inflammatory Pathway Blocking: Medicines like biologics and JAK inhibitors block specific proteins or enzymes that signal inflammation, such as tumor necrosis factor (TNF), interleukin-6 (IL-6), or Janus kinases. By interrupting these signals, they reduce joint inflammation and associated damage.
Cellular Level Action: Some medications work at the cellular level by affecting immune cell production, activation, or lifespan, helping to reduce the number of cells that contribute to joint inflammation.
Symptom Relief Mechanisms: NSAIDs and corticosteroids work more quickly by reducing inflammation and blocking pain signals, providing relief while disease-modifying drugs take effect over weeks to months.
The goal of treatment is not just symptom relief but achieving remission or low disease activity, which helps prevent irreversible joint damage and disability.
Who May Benefit From This Category?
Healthcare providers may prescribe rheumatoid arthritis medicines to:
Newly Diagnosed Patients: Individuals recently diagnosed with RA typically begin treatment promptly to prevent early joint damage and achieve better long-term outcomes.
Patients With Active Disease: Those experiencing ongoing joint inflammation, pain, swelling, or stiffness that affects daily activities and quality of life.
Individuals With Progressive RA: Patients showing signs of disease progression, including new joint involvement, increased inflammatory markers, or radiographic evidence of joint erosion.
Those Not Responding to Initial Treatment: Patients who have tried first-line medications without adequate response may benefit from alternative DMARDs, biologics, or combination therapy approaches.
People Seeking Disease Remission: Patients working with their rheumatologist to achieve and maintain low disease activity or remission through optimized medication regimens.
Treatment decisions are highly individualized and based on disease activity, prognostic factors, patient preferences, comorbidities, and previous treatment responses. Only qualified healthcare professionals can determine appropriate treatment for each patient.
Important Safety Information:-
Rheumatoid arthritis medications require careful medical supervision due to their significant effects on the immune system:
Infection Risk: Many RA medications reduce immune system activity, which can increase susceptibility to infections. Patients should be screened for latent tuberculosis and hepatitis before starting treatment, maintain up-to-date vaccinations (avoiding live vaccines on some treatments), and promptly report signs of infection.
Liver and Kidney Monitoring: Regular blood tests are essential for many RA medications to monitor liver function, kidney function, and blood cell counts, as some drugs can affect these systems.
Contraindications: Certain patients should avoid specific RA medications, including those with active infections, certain cancers, severe heart failure, demyelinating diseases, or during pregnancy and breastfeeding for many agents.
Drug Interactions: RA medications can interact with other medicines, including over-the-counter drugs and supplements. Always inform all healthcare providers about your complete medication list.
Pregnancy Planning: Many RA medications are not safe during pregnancy and require discontinuation before conception. Women of childbearing potential should discuss family planning with their rheumatologist well in advance.
Skin Cancer Screening: Some immunosuppressive medications may increase skin cancer risk, making regular dermatological examinations important.
Never start, stop, or change RA medications without direct consultation with your prescribing physician, as sudden discontinuation can lead to disease flares and potential complications.
Usage Guidance (General):-
Proper medication use is critical for rheumatoid arthritis treatment success:
Dosing Schedules: RA medications have varied dosing schedules—some are taken daily, others weekly, and biologics may be administered every few weeks or months by injection or infusion. Strict adherence to the prescribed schedule is essential for maintaining disease control.
Administration Methods: Depending on the specific medication, administration may involve oral tablets, subcutaneous injections (which patients can often self-administer after training), or intravenous infusions given in a clinic or hospital setting.
Time to Effect: Disease-modifying drugs typically require weeks to months to show full benefit. Patients should continue treatment as prescribed, even if immediate improvement isn’t apparent, while maintaining communication with their healthcare team.
Combination Therapy: Many patients take multiple medications simultaneously, such as a DMARD combined with a biologic, or symptomatic treatments alongside disease-modifying therapy. Each medication serves a specific purpose in the overall treatment strategy.
Missed Doses: If a dose is missed, patients should follow their healthcare provider’s specific instructions rather than doubling up or making assumptions about catch-up dosing.
Medication Adjustments: Rheumatologists regularly assess treatment effectiveness and may adjust doses, switch medications, or modify combinations based on disease activity, side effects, and treatment goals.
All usage decisions must be made by qualified healthcare professionals who can monitor treatment effectiveness and safety through regular clinical assessments and laboratory testing.
Side Effects & Risks (General Overview):-
Rheumatoid arthritis medications can cause various side effects, which vary by drug class and individual patient factors:
Common Side Effects: Patients may experience nausea, digestive upset, headache, injection site reactions, fatigue, or minor increases in infection susceptibility. Many side effects are manageable and may decrease over time as the body adjusts.
Gastrointestinal Effects: Some medications, particularly methotrexate and NSAIDs, can cause stomach upset, mouth sores, or digestive discomfort. Taking medications with food or using supplemental folic acid may help in certain cases.
Serious Infections: Because these medications affect immune function, serious bacterial, viral, or fungal infections can occur and require immediate medical attention. Warning signs include fever, persistent cough, unusual fatigue, or wound healing problems.
Liver Function Changes: Some RA medications can affect liver enzymes, requiring regular blood test monitoring. Most changes are mild and reversible, but occasional patients may need medication adjustments or discontinuation.
Blood Cell Changes: Certain medications can affect white blood cell, red blood cell, or platelet counts, making regular blood monitoring essential for early detection and management.
Infusion and Injection Reactions: Biologic medications may cause reactions during infusion or at injection sites, ranging from mild redness to more significant allergic-type responses requiring medical management.
Cardiovascular Considerations: Some medications may affect blood pressure, cholesterol, or cardiovascular risk profiles, particularly in patients with pre-existing heart conditions.
Patients should maintain open communication with their healthcare team about any new symptoms or concerns. Many side effects can be effectively managed without discontinuing treatment, but medical guidance is essential for safe decision-making.
Choosing the Right Medicine:-
Selecting appropriate rheumatoid arthritis treatment is a collaborative process between patients and healthcare professionals:
Individual Disease Assessment: Rheumatologists consider disease severity, activity level, presence of poor prognostic factors (such as high antibody levels or early erosions), and rate of progression when recommending specific treatments.
Patient-Specific Factors: Treatment selection accounts for age, comorbidities, other medications, lifestyle factors, pregnancy plans, and individual preferences regarding oral versus injectable medications.
Treatment Goals: The primary goal is achieving remission or low disease activity, which requires regular monitoring and potentially adjusting therapy if targets aren’t met within appropriate timeframes.
Response Monitoring: Healthcare providers use clinical assessments, patient-reported outcomes, inflammatory markers, and imaging studies to evaluate treatment effectiveness and guide adjustments.
Risk-Benefit Discussion: Each medication carries specific benefits and risks. Rheumatologists help patients understand these tradeoffs and make informed decisions aligned with their values and circumstances.
Sequential Therapy Approach: Treatment often begins with conventional DMARDs, progressing to biologics or JAK inhibitors if needed. Some patients with severe disease may start with combination therapy or advanced medications from the outset.
Cost and Access Considerations: Healthcare teams can discuss medication costs, insurance coverage, patient assistance programs, and biosimilar options when relevant to treatment decisions.
Never select or switch RA medications based on online information, peer recommendations, or personal research alone. These are powerful medications requiring professional medical management for safe and effective use.
Storage & Handling Advice:-
Proper storage ensures medication effectiveness and safety:
Refrigeration Requirements: Many biologic medications require refrigeration between 2°C and 8°C (36°F to 46°F). They should never be frozen and must be discarded if freezing occurs. Allow refrigerated medications to reach room temperature before injection for improved comfort.
Room Temperature Storage: Oral medications are typically stored at room temperature in a dry location away from moisture, heat, and direct sunlight. Bathrooms are generally not ideal storage locations due to humidity.
Light Protection: Some medications come in light-protective packaging or amber bottles and should remain protected from bright light to maintain stability.
Original Packaging: Keep medications in original containers with intact labels showing prescription information, expiration dates, and specific storage instructions.
Traveling With Medications: When traveling, particularly with biologics, use insulated cooler bags with ice packs (avoiding direct contact between medication and ice), and carry medications in hand luggage rather than checked baggage when flying.
Injection Supplies: If self-administering injections, store supplies safely, dispose of needles and syringes in approved sharps containers, and never reuse injection equipment.
Child Safety: Store all medications securely out of reach of children and pets, preferably in locked cabinets, as accidental ingestion could cause serious harm.
Expiration Dates: Check expiration dates regularly and never use expired medications. Consult your pharmacist about proper disposal methods for unused or expired medications.
Injectable Medication Inspection: Before each use, visually inspect injectable biologics for particles, cloudiness, or discoloration. Do not use if the solution appears abnormal.
Frequently Asked Questions (Category-Based)?
How long does it take for rheumatoid arthritis medications to work?
The time to noticeable improvement varies significantly by medication type. Conventional DMARDs like methotrexate typically require 6-12 weeks before substantial benefits appear, with full effects sometimes taking 3-6 months. Biologic medications may show some improvement within 2-4 weeks, with maximum benefit at 12-16 weeks. Corticosteroids work much faster, often within days, which is why they’re sometimes used as bridge therapy while waiting for disease-modifying drugs to take effect. JAK inhibitors can produce relatively rapid responses, sometimes within 2-4 weeks. It’s important to continue medications as prescribed during this initial period and maintain regular follow-up appointments so your rheumatologist can assess response and adjust treatment if necessary.
Can I stop taking my medication if my symptoms improve?
No, you should never stop rheumatoid arthritis medications without consulting your rheumatologist, even if you feel significantly better. RA is a chronic condition requiring ongoing treatment to maintain remission and prevent disease flares and joint damage. When symptoms improve or disappear, it’s typically because the medication is working effectively, not because the disease has resolved. Stopping treatment often leads to disease reactivation, sometimes causing more severe inflammation than before. If you’ve achieved sustained remission, your doctor may consider carefully reducing medication doses (called dose tapering) under close supervision, but this decision should only be made by your healthcare team based on objective measures of disease activity, not just symptom relief.
Are biologic medications safe for long-term use?
Biologic medications have been used for over two decades with extensive safety monitoring, and many patients take them safely for years. Long-term studies show that while biologics do increase infection risk and require ongoing monitoring, most patients tolerate them well with appropriate medical supervision. The key to safe long-term use includes regular health monitoring through blood tests and clinical assessments, staying current with appropriate vaccinations before starting treatment, promptly reporting any infections or health changes, and maintaining honest communication with your healthcare team about any concerns. The benefits of preventing joint damage and maintaining quality of life typically outweigh the risks for most patients, but this balance should be regularly reassessed with your rheumatologist based on your individual circumstances and disease course.
What should I do if I experience side effects from my medication?
The appropriate response depends on the severity and type of side effect. For mild effects like slight nausea, temporary fatigue, or minor injection site redness, contact your healthcare provider’s office for guidance—these may be manageable without medication changes. For moderate symptoms that affect daily activities or persist beyond a few days, schedule an appointment with your rheumatologist to discuss whether dose adjustment or medication change is needed. For serious symptoms, including signs of infection (fever, persistent cough, unusual fatigue), severe allergic reactions (difficulty breathing, significant swelling, widespread rash), unusual bleeding or bruising, severe abdominal pain, or yellowing of skin or eyes, seek immediate medical attention. Never stop RA medications abruptly without medical guidance, as this can trigger disease flares. Keep a symptom diary to help your healthcare team identify patterns and make informed treatment adjustments.
Medical Disclaimer:-
This content is provided for general educational and informational purposes only and is not intended to substitute for professional medical advice, diagnosis, or treatment. Rheumatoid arthritis is a complex chronic condition requiring individualized management by qualified rheumatologists and healthcare professionals.
The information presented represents general category-level guidance and cannot account for individual patient circumstances, specific medication formulations, drug interactions, comorbidities, or the latest clinical research and treatment guidelines. Every patient’s condition, treatment needs, and response to therapy are unique.
Never start, stop, adjust, or change rheumatoid arthritis medications without direct consultation with your prescribing physician. Self-medication and treatment modifications can lead to serious health consequences,s including disease flares, irreversible joint damage, medication complications, and dangerous side effects.
If you experience symptoms suggesting rheumatoid arthritis or any concerning health changes while on RA medications, consult with a qualified healthcare provider promptly. In case of medical emergencies, including signs of serious infection, severe allergic reactions, or other acute symptoms, seek immediate emergency medical care.
Always discuss your complete medical history, current medications, supplements, and health concerns with your healthcare team before starting any new treatment. Treatment decisions should be made collaboratively between patients and their rheumatology care team based on comprehensive medical evaluation, current clinical guidelines, and individual patient values and preferences.
This information does not endorse or recommend any specific medication, treatment approach, or healthcare provider, nor does it represent the most current research or clinical practice standards. Healthcare information evolves continuously, and treatment recommendations may change based on new evidence and individual patient responses.
-
Cyclophil Me 25mg (Cyclosporine)
Active Ingredient Cyclosporine Manufacturer Biocon Limited Packaging 5 capsules in 1 strip, 6 capsules in 1 strip Strength 25mg, 50mg, 100mg Delivery Time 6 To 15 days SKU: Cyclophil Me 25mg (Cyclosporine) Price range: $21.00 through $200.00Cyclophil Me 25mg (Cyclosporine)
Price range: $21.00 through $200.00 -
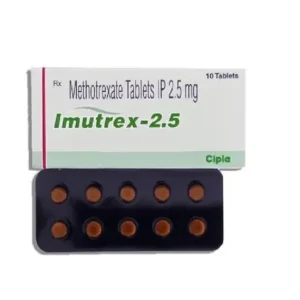
Imutrex 2.5 Mg (Methotrexate)
Active Ingredient Methotrexate Manufacturer Cipla Limited Packaging 10 tablets in 1 strip Strength 2.5 Mg, 7.5 Mg, 10 Mg Delivery Time 6 To 15 days SKU: Imutrex 2.5 Mg (Methotrexate) Price range: $27.00 through $195.00Imutrex 2.5 Mg (Methotrexate)
Price range: $27.00 through $195.00 -
Lefumide 10 Mg (Leflunomide)
Active Ingredient Leflunomide Manufacturer Cipla Limited Packaging 10 tablets in 1 strip Strength 10 Mg Delivery Time 6 to 15 days SKU: Lefumide 10 Mg (Leflunomide) Price range: $28.00 through $201.00Lefumide 10 Mg (Leflunomide)
Price range: $28.00 through $201.00